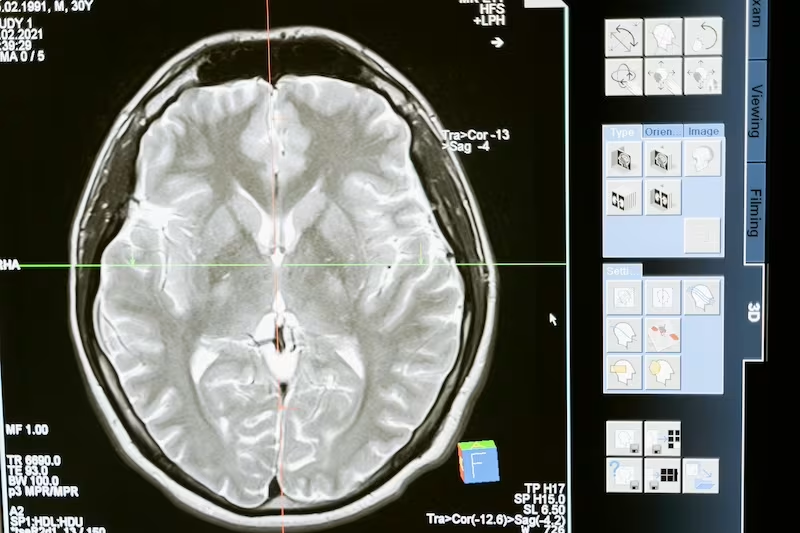
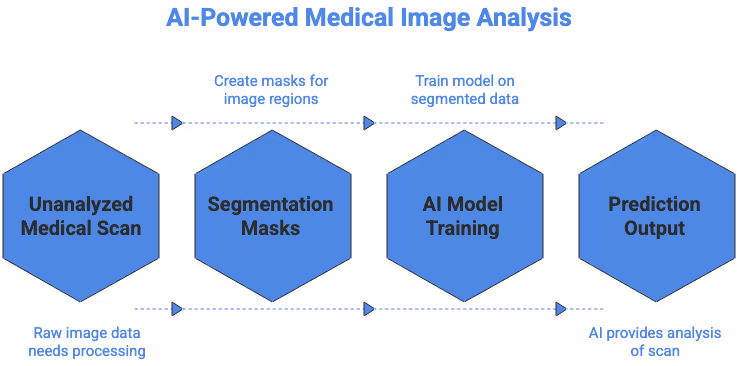
Medical image segmentation has become a cornerstone of modern healthcare AI, supporting clinical diagnosis, treatment planning, and medical research at unprecedented scale. As hospitals generate vast quantities of CT, MRI, PET, ultrasound, X-ray, and pathology images, segmentation transforms raw scans into structured, clinically meaningful regions. These regions allow clinicians and machine learning systems to quantify abnormalities, track disease progression, and support improved patient outcomes.
Segmentation is also foundational to supervised deep learning. Models cannot learn reliably without high quality segmentation masks that accurately represent anatomical or pathological structures. When segmentation is consistent and clinically validated, AI systems become more accurate and reliable. When segmentation is noisy or inconsistent, model performance deteriorates. This article explores what segmentation is, why it matters, how it is performed, and the challenges faced by teams building clinical-grade datasets.
Understanding the Importance of Medical Image Segmentation in Modern Healthcare
Medical imaging supports nearly every area of medicine, but the complexity of modern scans makes interpretation increasingly demanding. Medical image segmentation enables clinicians and AI systems to isolate and analyze specific regions such as tumors, lesions, organs, or vascular structures. By outlining these areas, segmentation helps clinicians focus on relevant regions and supports standardized measurements across time and individuals.
This structure is central to quantitative imaging. Instead of relying solely on subjective interpretation, segmentation enables objective, reproducible measurements. In oncology, for example, segmentation supports tumor volume analysis, helps evaluate treatment response, and improves consistency between radiologists. For surgeons, segmentation enhances preoperative planning by visualizing anatomy in three dimensions. For AI developers, segmentation provides highly informative labels that allow models to learn relevant visual patterns.
The rising demand for AI-driven diagnostics and decision support systems makes segmentation even more critical. Hospitals, startups, and research teams depend on segmentation to train systems that can operate safely in real clinical environments.
What Is Medical Image Segmentation
Medical image segmentation is the process of dividing a medical scan into anatomically or pathologically meaningful structures. Each pixel or voxel is assigned a label that corresponds to a region of interest. These regions may include organs, lesions, tumors, tissue types, or vascular networks. Segmentations can be binary (single structure) or multi-class (multiple structures).
Creating accurate segmentation masks requires specialized knowledge. Many structures have ambiguous borders or appear differently depending on the imaging modality. For example, the same brain tumor can present radically different contrasts in CT versus MRI. This means segmentation workflows must be supported by clinical expertise, clear guidelines, and robust quality control. The accuracy of these masks directly influences the reliability of downstream AI systems.
Segmentation also supports a wide range of healthcare analytics. From volumetric measurements to biomechanical simulations, segmentation forms the basis for deeper quantitative analysis. This makes it one of the most valuable components of medical imaging workflows today.
For example, the National Institutes of Health maintains one of the largest biomedical imaging research hubs in the world where many datasets rely heavily on segmentation for ground truth labeling.
Why Medical Image Segmentation Matters for AI Systems
AI systems learn by identifying patterns in data. Segmentation provides the precise pixel-level labels needed to train deep learning models to recognize complex structures. Without segmentation, models cannot reliably distinguish between normal and abnormal regions or quantify disease progression.
Segmentation improves AI systems by:
• enabling earlier disease detection
• supporting reproducible measurements
• reducing radiologist workload
• improving model explainability
• enhancing treatment planning
For example, segmentation masks help AI models detect lung nodules, measure liver tumors, or isolate brain structures for neurosurgical planning. Segmentation also strengthens regulatory approval pathways. Agencies such as the FDA require rigorous evidence of model performance, generalization, and safety. High-quality segmentation data provides the foundation for this evidence.
Segmentation also helps reduce cognitive load for clinicians. Automated segmentation tools can quickly outline anatomy, allowing radiologists to focus on interpretation rather than manual tracing. When used responsibly, segmentation accelerates workflows while maintaining clinical accuracy.
Medical Image Segmentation also influences regulatory approval. Agencies such as the FDA require evidence that medical AI systems behave predictably across populations, scanners, and imaging protocols. Without strong segmentation data, these requirements become difficult to meet.
Medical Image Segmentation Methods Used Today
Medical image segmentation has evolved significantly. Today’s workflows combine expert knowledge with machine intelligence to create segmentation masks efficiently and reliably.
Manual Segmentation
Manual segmentation involves experts outlining structures by hand on each slice of a scan. This method remains the gold standard for accuracy. Radiologists, biomedical engineers, or trained annotators trace boundaries of organs, lesions, or tissues with meticulous precision. Manual segmentation is essential for uncommon pathologies, irregular tumors, or multimodal imaging.
Although time consuming, manual segmentation sets the foundation for ground-truth labels. These annotations are used to evaluate automated models and calibrate semi-automatic tools. Even as AI advances, manual review continues to play a crucial role in maintaining dataset quality and clinical safety.
Semi-Automatic Segmentation
Semi-automatic segmentation blends algorithmic assistance with human oversight. Techniques such as region growing, thresholding, or active contours generate preliminary masks that annotators refine. This approach accelerates annotation while maintaining high accuracy.
Semi-automatic tools are especially useful for segmenting organs with well-defined shapes or high contrast boundaries. They reduce fatigue for annotators and increase consistency across large datasets. This method is a practical middle ground when full automation is not yet reliable enough for clinical workflows.
Fully Automated Deep Learning Segmentation
Deep learning has reshaped segmentation. Models such as U-Net, nnU-Net, and transformer-based architectures can automatically generate masks for complex structures. These models analyze large datasets to learn the visual patterns associated with organ and lesion boundaries.
Automated segmentation dramatically reduces annotation time and supports large-scale studies. However, automated systems require high quality training data, careful evaluation, and ongoing monitoring. Research platforms such as Grand Challenge showcase cutting-edge segmentation models used across the medical imaging community.
Key Applications of Medical Image Segmentation in Healthcare
Segmentation underpins many of the most impactful clinical AI use cases. Below are some of the primary domains where segmentation drives value.
Tumor and Lesion Detection
In oncology, segmentation is essential for identifying tumors and tracking them across time. Segmentation allows clinicians to measure tumor volume, assess margins, and monitor treatment response with quantitative precision. AI models trained on segmented tumors can support earlier detection and reduce variability between radiologists. This capability is particularly important for diseases such as liver cancer, gliomas, lung nodules, and metastatic lesions. AI Teams often refer to resources such as The Cancer Imaging Archive.
Organ and Tissue Segmentation
Organ segmentation supports surgical planning, radiation therapy, and disease monitoring. For example, liver segmentation is crucial for preoperative volume calculation, while heart segmentation enables functional assessment in cardiology.
AI systems are increasingly used to automate organ segmentation, helping radiology teams process scans more efficiently and consistently. These tools reduce manual workload and ensure greater reproducibility across cases.
Vascular and Blood Flow Analysis
Vessel segmentation reveals stenosis, aneurysms, and other vascular abnormalities. It supports critical workflows in neurosurgery, cardiology, and stroke care. High-quality vessel segmentation also enables 3D reconstructions and blood flow simulations that inform clinical decisions.
Because vessels can be small and branching, segmentation requires domain expertise and robust algorithms. Vascular segmentation remains a highly active area of research.
Radiotherapy Planning
Radiation oncologists rely on segmentation to outline organs at risk and target regions. Accurate contouring ensures radiation is delivered precisely while minimizing damage to surrounding tissues. Automated segmentation tools help reduce variability in clinical practice and accelerate treatment planning.
Segmentation is essential for head and neck cancers, prostate cancer, and thoracic tumors. High-quality segmentation enhances both safety and therapeutic effectiveness.
Surgical Navigation and Robotics
Segmentation enables high-resolution 3D models that guide surgeons during minimally invasive or robotic procedures. These models help clinicians visualize structures clearly and avoid complications. Real-time segmentation supports intraoperative decision making and improves surgical outcomes.
As robotic systems become more advanced, segmentation will continue to play a central role in surgical navigation and automation.
Pathology and Cell Segmentation
Digital pathology requires segmentation of cells, nuclei, and tissue regions. Whole slide images often exceed gigapixel resolution, making manual analysis impractical. Automated segmentation helps pathologists focus on clinically relevant regions and supports tasks such as cancer grading and biomarker discovery.
Segmentation is also fundamental to computational pathology, where machine learning models analyze cellular patterns for diagnostic insight.
Challenges Faced When Developing Segmentation Models
Building reliable segmentation models requires navigating several technical, clinical, and regulatory challenges.
Limited Labeled Data
High-quality segmentation datasets are difficult to obtain. Annotation requires clinical expertise, is time intensive, and must follow strict guidelines. Many hospitals cannot allocate enough radiologists or specialists to produce large volumes of labeled data. As a result, AI teams often face shortages of high-quality segmentation masks.
This scarcity limits model generalization and slows development timelines. It also makes rare diseases particularly challenging to model.
Variability in Imaging Modalities
Different modalities such as CT, MRI, PET, and ultrasound produce images with very different textures, contrasts, and noise patterns. Even within a single modality, variations in scanners, acquisition protocols, slice thickness, and reconstruction algorithms create significant differences in appearance.
These variations introduce domain shift, which makes it harder for models trained on one dataset to perform well on another. Successful segmentation models must account for this variability through robust training strategies.
Annotation Complexity
Some structures are extremely difficult to segment accurately. Tumor boundaries may be irregular or poorly defined. Small lesions may be easy to miss. Vessels may blend into surrounding tissue. Even expert annotators may disagree, leading to inter-observer variability.
This complexity demands clear guidelines, expert reviewers, and multiple layers of quality control. Without these safeguards, datasets become inconsistent, reducing model performance.
Domain Shift Across Hospitals
Datasets from different institutions vary significantly in patient demographics, scanner hardware, and imaging protocols. A model trained on one hospital’s scans might fail when deployed elsewhere. Mitigating domain shift requires multi-site datasets, harmonization techniques, or domain adaptation methods.
This challenge is one of the primary obstacles to deploying AI segmentation tools in real clinical practice.
Regulatory and Ethical Considerations
Segmentation models used clinically must comply with strict regulatory standards such as HIPAA. Agencies such as the FDA require evidence that models are accurate, reliable, and fair across populations. Segmentation errors can directly impact diagnosis or treatment, so regulatory oversight is essential.
Ethical considerations include patient privacy, informed consent, and dataset governance. Teams must ensure segmentation workflows uphold these principles at every stage.
Future Trends in Medical Image Segmentation
Rapid advancements in AI promise to reshape the future of medical image segmentation. Several trends are already influencing how hospitals and research labs approach imaging.
Foundation Models Trained on Large Multimodal Medical Data
Foundation models are beginning to transform medical imaging. These models are trained on vast collections of multi-modality scans and can generalize across tasks with minimal fine-tuning. They allow clinicians to perform segmentation even with limited training data. The open research community, including the MICCAI Society continues to drive innovation in this space.
Federated Learning
Federated learning enables collaborative model training across hospitals without sharing raw data. This protects privacy and expands dataset diversity, helping models generalize more effectively. Federated segmentation workflows are especially promising for rare diseases.
3D and 4D Segmentation
Advances in deep learning now support volumetric (3D) and temporal (4D) segmentation. These approaches are essential for tasks such as cardiac function analysis, respiratory movement study, and dynamic MRI. As computing power increases, 3D and 4D segmentation will become more accessible.
Cross Modality Fusion
Combining information from multiple imaging modalities improves segmentation accuracy and reduces ambiguity. CT, MRI, and PET each provide unique insights, and multimodal fusion helps models capture richer context. Cross-modality segmentation is particularly valuable in oncology and neurology.
Real Time Clinical Integration
Segmentation tools are increasingly integrated into PACS, surgical robots, and real-time imaging platforms. These systems support fast decision making and improve workflow efficiency. Real-time segmentation is expected to become a standard feature in advanced imaging environments.
If You Are Building a Segmentation Project
Whether you are a hospital, research lab, or AI startup, success depends on the quality and consistency of your segmentation pipeline. Common questions to consider include:
- Which medical image segmentation methods best fit your imaging modality
- How to source enough annotated scans
- How to validate segmentation consistency
- How to prepare data for regulatory submission
- How to outsource segmentation safely while maintaining clinical quality
Organisations increasingly rely on experienced annotation partners to handle clinical scale labeling with expert supervision.
Ready to Advance Your Medical Imaging AI Project : Contact us at DataVLab
If you are planning to build or scale a medical image segmentation project and want reliable, expert supported annotation, we would be glad to help. At DataVLab, we specialize in high accuracy healthcare datasets with medically trained annotators, strict quality control, and scalable production workflows.
Reach out anytime and tell us what you are working on. We would be happy to help you move your project forward.