Introduction: Why Medical Image Annotation Matters in the AI Age
The intersection of artificial intelligence and healthcare is transforming modern medicine. From early cancer detection to robotic surgery assistance, AI’s potential is immense—but it all starts with data. Specifically, annotated medical images.
Medical image annotation is the backbone of supervised learning in healthcare AI. It enables models to “see” what experts see—tumors, fractures, lesions, anomalies—and learn to recognize patterns across vast amounts of clinical data. But unlike natural images, annotating medical scans presents high stakes, unique challenges, and a need for deep domain expertise. According to the National Institutes of Health, access to large, annotated datasets is critical for developing AI tools in healthcare.
This comprehensive guide explores the modalities, tools, and real-world use cases that define medical image annotation today. Whether you're building a deep learning model for radiology or managing a hospital AI project, this article equips you with the insight needed to make informed, strategic decisions.
1. Understanding Medical Image Annotation
What Is Medical Image Annotation?
Medical image annotation is the process of labeling visual data from diagnostic imaging (like X-rays or MRIs) to make it understandable to machine learning algorithms. This involves marking structures, regions of interest (ROIs), pathologies, or abnormalities using various techniques—bounding boxes, contours, segmentation masks, and more.
Why It’s Crucial for AI Models
- Supervised learning needs ground truth to learn from.
- Helps AI systems detect, classify, and even predict health conditions.
- Reduces diagnostic time and variability between physicians.
- Improves model accuracy, sensitivity, and generalizability.
Who Performs Medical Annotations?
- Radiologists & Pathologists: For high-complexity images and clinical validation.
- Specialized annotators: Trained medical professionals or biologists.
- Annotation vendors: Companies offering managed services with QA pipelines.
2. Key Modalities in Medical Image Annotation
Medical imaging spans a diverse set of modalities, each with unique properties and annotation challenges.
🩻 2.1. X-rays
- Use Case: Chest X-rays for pneumonia, fractures, TB, or COVID-19 detection.
- Annotation Types: Bounding boxes around lesions or opacity; segmentation of organs (lungs, heart).
- Challenges: Low contrast, overlapping structures, variability in projection.
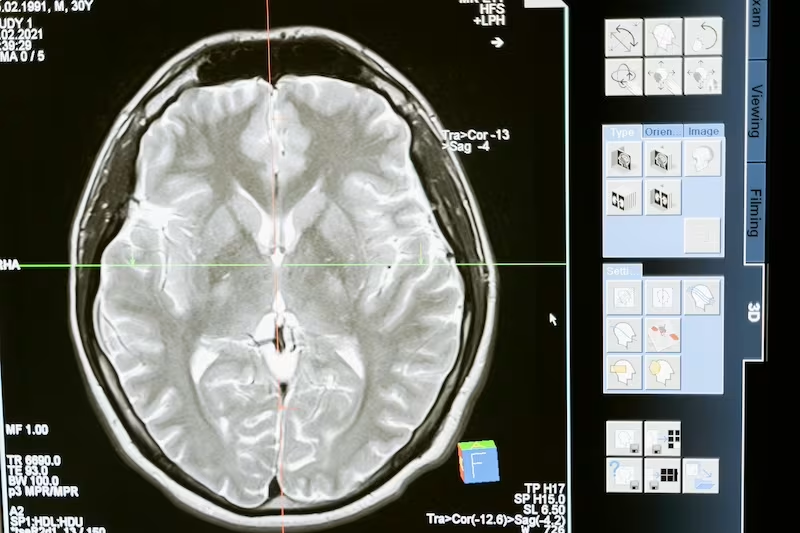
🧲 2.2. MRI (Magnetic Resonance Imaging)
- Use Case: Brain tumors, spinal cord analysis, knee cartilage tracking.
- Annotation Types: Multi-slice segmentation, 3D reconstruction.
- Challenges: Large file sizes, non-standard orientations, DICOM complexities.
⚛️ 2.3. CT Scans (Computed Tomography)
- Use Case: Lung nodule detection, liver segmentation, trauma triage.
- Annotation Types: Volumetric annotations, 3D bounding boxes, masks.
- Challenges: High dimensionality, contrast variations, radiation artifacts.
🧪 2.4. Pathology Slides (WSI)
- Use Case: Cancer grading, cell counting, nucleus segmentation.
- Annotation Types: Polygonal outlines, pixel-level masks, heatmaps.
- Challenges: Gigapixel resolution, need for precision at cellular scale.
🧠 2.5. Ultrasound
- Use Case: Fetal measurements, cardiac echo, thyroid nodule classification.
- Annotation Types: Line measurements, ROI masks, anatomical labeling.
- Challenges: Operator dependence, image noise, variable angles.
👁️ 2.6. Ophthalmology (Fundus, OCT)
- Use Case: Diabetic retinopathy, glaucoma, macular degeneration.
- Annotation Types: Layer segmentation, lesion labeling.
- Challenges: Subtle contrast differences, layer overlaps.
🧬 2.7. Nuclear Medicine (PET, SPECT)
- Use Case: Functional imaging for cancer staging, Alzheimer’s detection.
- Annotation Types: Activity thresholding, fused image labeling (PET/CT).
- Challenges: Multimodal registration, functional vs. structural fusion.
3. Common Annotation Techniques for Medical Imaging
Medical imaging requires annotation techniques that are both clinically accurate and computationally efficient. The right technique depends on the task—be it detecting an organ, segmenting a tumor, or classifying an entire scan. Below are the most widely used annotation methods in healthcare AI workflows.
🟩 3.1. Semantic Segmentation
What it is:
Semantic segmentation involves labeling every pixel in an image based on its class (e.g., tumor, healthy tissue, bone). All pixels belonging to the same category receive the same label.
Where it's used:
- Tumor segmentation in MRI or CT scans
- Organ delineation in radiotherapy planning
- Tissue classification in histopathology slides
Why it matters:
This technique provides the highest level of detail, making it essential for tasks where boundaries matter, such as differentiating between healthy and diseased tissue.
Best practices:
- Use multi-rater validation to account for medical ambiguity
- Apply class balancing techniques to avoid undertraining rare structures
- Consider active learning loops for continuous improvement
🟨 3.2. Bounding Boxes
What it is:
Rectangular boxes drawn around an object of interest, indicating its approximate location.
Where it's used:
- Lung nodule detection on chest X-rays
- Bone fracture identification in orthopedic scans
- Polyp detection in colonoscopy videos
Why it matters:
Bounding boxes are quick to annotate and ideal for early-stage model training or triage systems where precise contours are less critical.
Best practices:
- Ensure the box tightly encloses the object, avoiding excess background
- Use class labels for each box to distinguish between object types
- Combine with classification for improved diagnostic workflows
🔺 3.3. Polygon Annotation
What it is:
Flexible outlines drawn point-by-point around irregularly shaped structures, allowing more detailed boundary definitions than boxes.
Where it's used:
- Lesion annotation in dermatology or radiology
- Tumor borders in pathology or brain imaging
- Retinal vessels or hemorrhages in ophthalmology
Why it matters:
Polygons allow for precise modeling of object contours, which is crucial in medical contexts where even small misalignments can alter diagnoses or treatment plans.
Best practices:
- Annotate using a high-resolution interface to prevent oversimplified shapes
- Cross-check with segmentation masks when available
- Use zoom and pan tools for detailed tracing in large images (e.g., WSI)
🟦 3.4. Keypoint Annotation
What it is:
Keypoints are individual markers placed on specific anatomical landmarks or areas of interest.
Where it's used:
- Skeletal landmarks in orthopedics for posture or injury analysis
- Fetal biometry in ultrasound (crown-rump length, femur length)
- Facial features in cleft palate or surgical planning
Why it matters:
Keypoint annotation enables spatial and geometric analysis of body structures, useful for measuring growth, movement, or deformation.
Best practices:
- Maintain consistent labeling conventions across images and annotators
- Consider inter-rater variability for anatomical points with low visibility
- Use motion tracking if annotating keypoints in video sequences (e.g., cardiac echo)
🟥 3.5. Instance Segmentation
What it is:
Similar to semantic segmentation, but each object is labeled individually, even if they share the same class (e.g., labeling each cell in a cluster).
Where it's used:
- Nuclei detection in pathology slides
- Lung nodules or lesions in CT
- Detection of overlapping structures in ultrasound or mammograms
Why it matters:
Instance segmentation provides a granular level of detail, making it possible to count, measure, and analyze individual instances in a crowded field.
Best practices:
- Apply post-processing to separate touching instances
- Ensure annotations are validated with cell-level accuracy
- Ideal for use cases involving object density metrics (e.g., cell count, tumor multiplicity)
🧩 3.6. 3D Annotation
What it is:
Annotation performed across a volume of slices, such as in CT or MRI, creating a 3D representation of the target region.
Where it's used:
- Brain tumor segmentation across axial, coronal, sagittal planes
- Organ reconstruction (liver, lungs, kidneys)
- Orthopedic planning using 3D bone structures
Why it matters:
Most modern radiological workflows involve 3D data. Accurate 3D annotation allows for volumetric analysis, which is crucial for surgical planning, dose calculation, or monitoring disease progression.
Best practices:
- Use annotation tools with multi-planar reformatting (MPR)
- Align annotations across slices to ensure smooth 3D continuity
- Validate with volumetric accuracy metrics (e.g., Dice coefficient, IoU)
🧪 3.7. Classification Tags
What it is:
Assigning metadata or categorical labels to an entire image or series—without drawing shapes.
Where it's used:
- COVID-19 diagnosis from chest X-rays
- Cancer staging based on pathology reports
- Presence of comorbidities inferred from imaging patterns
Why it matters:
While less granular, classification tags are extremely useful for training image-level classifiers, managing datasets, and automating high-level triage decisions.
Best practices:
- Define clear and consistent class definitions (e.g., “mild”, “moderate”, “severe”)
- Combine with structured metadata (e.g., patient age, modality)
- Use for building weakly supervised learning pipelines when granular annotation is unavailable
4. Annotation Tools for Medical AI
Choosing the right annotation tool can dramatically affect speed, accuracy, and compliance.
🛠️ Key Features to Look For
- DICOM Support: For radiology and multi-slice data.
- Multiplanar Viewing: Annotate in axial, sagittal, coronal views.
- 3D Volume Rendering: Crucial for CT and MRI.
- HIPAA/GDPR Compliance: Especially when dealing with PHI.
- Built-in QA Workflows: Reviewer roles, inter-annotator agreement tracking.
- Pathology-Specific Features: Zooming, cell-level tagging, WSI handling.
🧰 Popular Annotation Platforms: Encord, Labelbox, CVAT+OHIF, MD.AI, etc.
5. Use Cases Across Healthcare Specialties
🧠 5.1. Radiology
AI models trained on annotated X-rays, CTs, and MRIs are now used for:
- Chest X-ray triage
- Lung cancer screening
- Brain tumor segmentation
- Fracture detection in trauma centers
Key Benefits: Faster diagnosis, reduced radiologist fatigue, improved consistency.
The RSNA has curated AI resources to support radiologists exploring deep learning and annotation use cases.
🦠 5.2. Pathology
Digital pathology annotation powers:
- Cancer grading systems
- Cell segmentation and classification
- Mitotic figure detection
- Rare disease biomarker analysis
Key Tools: WSI annotation, stain normalization, high-resolution tiling.
👁️ 5.3. Ophthalmology
Image annotation in fundus and OCT imaging is used to:
- Detect diabetic retinopathy
- Grade glaucoma severity
- Monitor macular thickness over time
Real-world Example: Google’s DeepMind algorithm for DR screening in India.
🤍 5.4. Cardiology
Echocardiogram annotations help train models to:
- Identify left ventricular function
- Detect valvular defects
- Measure ejection fraction automatically
Annotation of ultrasound videos is complex and requires temporal consistency.
🧬 5.5. Oncology
Multi-modal annotation supports:
- Tumor detection across imaging types
- Radiomics analysis for treatment planning
- Survival prediction models
Common Annotation Needs: Tumor size, location, stage, and progression.
🏥 5.6. Emergency & Trauma
AI systems are being built to rapidly identify:
- Pneumothorax
- Internal bleeding
- Spinal injuries
- Fractures in extremities
Annotations here must be fast, accurate, and auditable.
🧪 5.7. Drug Discovery & Clinical Trials
In early drug development, annotation supports:
- Biomarker tracking
- Disease progression mapping
- AI-powered eligibility screening
Imaging endpoints now often rely on semi-automated labeling reviewed by clinicians.
6. Quality Assurance in Medical Annotation
Why QA Is Non-Negotiable
A small annotation error can result in:
- False positives or negatives
- Regulatory issues in clinical AI deployment
- Decreased trust among physicians
Proven QA Strategies
- Double-blind reviews
- Inter-annotator agreement (IAA) scoring
- Gold-standard datasets for benchmarking
- Model-in-the-loop validation
Annotation vendors must implement rigorous multi-layer QA processes to ensure clinical-grade outputs.
7. Challenges in Medical Image Annotation
🧠 Expertise Gap
High-quality annotation often requires specialist medical knowledge, limiting scalability.
🔐 Data Privacy
Sensitive patient data must comply with GDPR, HIPAA, and local regulations.
📊 Class Imbalance
Rare diseases and conditions make it hard to build balanced datasets.
⚙️ Tool Limitations
Many general annotation tools lack support for DICOM, 3D, or WSI formats.
💰 Cost & Time
Expert annotation is expensive and time-consuming—project timelines must reflect this.
8. The Future of Medical Image Annotation
Model-Assisted Annotation (ML-in-the-Loop)
Trained AI models can suggest labels to speed up annotation, which are then verified by humans.
Synthetic Data & Augmentation
To solve data scarcity, synthetic medical images (via GANs or Sim2Real) are increasingly used in training pipelines.
Federated Annotation
Annotation workflows that stay on-premise at hospitals, without moving patient data to the cloud.
Interoperability Standards
New efforts like MONAI, DICOMweb, and FHIR are making annotation pipelines more integratable.
Conclusion: Data Quality is the Foundation of AI in Healthcare
Medical image annotation is more than just labeling pixels—it’s translating human clinical expertise into machine-readable insight. The success of any AI system in healthcare depends on how well its training data captures reality. That means accurate, high-quality, and ethically managed annotations, across every imaging modality and clinical use case.
As AI becomes standard in diagnosis, treatment, and monitoring, annotation will only grow in importance. Whether you're a healthtech innovator, AI researcher, or medical data manager—now is the time to invest in better data.
🔔 Partner with Experts in Medical Image Annotation
Need high-quality medical image annotation for your AI project?
Collaborate with DataVLab to ensure precise, clinical-grade annotations across all imaging modalities—radiology, pathology, ophthalmology, and more.
✅ DICOM-native annotation tools
✅ HIPAA/GDPR-compliant data handling
✅ Radiologist-led quality assurance
📩 Contacts us to learn how we can support your healthcare AI solution with expert-labeled medical data.
📬 Questions or projects in mind? Contact us